What is ED? A No-Nonsense, 2-Minute Breakdown
Erectile dysfunction (ED) is the persistent inability to get or keep an erection firm enough for sexual activity.
322 million men will silently deal with erectile dysfunction in 2025. According to the Cleveland Clinic, an estimated 52% of men experience some form of ED, with prevalence increasing with age.
If left untreated, ED can harm your confidence, relationships, and may even point to more serious health problems like heart disease.
This guide explains what ED is, what causes it, and how you can overcome it with proven, practical solutions.
Understanding Erectile Dysfunction (ED)
Let’s break down ED in plain language, what it means, how it’s medically defined, and the different ways it can show up in men’s lives.
What Is Erectile Dysfunction?
Erectile dysfunction is the persistent inability to achieve or maintain an erection sufficient for satisfying sexual activity.
It becomes medically relevant when this difficulty occurs frequently and impacts a person’s quality of life.
Medical Definition of ED
ED is clinically defined as “the consistent or recurrent inability to attain and/or maintain a penile erection sufficient for sexual intercourse” over a sustained period, typically several months.
Types of Erectile Dysfunction
ED isn’t one-size-fits-all; here’s how it shows up differently depending on the root cause or context.
Primary ED
Primary ED refers to men who have never been able to achieve or maintain an erection since the beginning of their sexual life.
It is rare and usually stems from deep-rooted psychological barriers, severe hormonal imbalances, or congenital physical abnormalities in the penis or pelvic region.
Treatment often involves psychological counseling and a thorough medical evaluation.
Secondary ED
Secondary ED is when a man previously had normal erectile function but later begins to experience difficulties.
This is the most common form of ED and is often caused by physical issues like high blood pressure, diabetes, obesity, or side effects from medications.
Emotional stress or anxiety may contribute as well. Fortunately, this type is usually treatable with lifestyle changes, medication, or therapy.
Situational ED
Situational ED occurs only under specific conditions, such as with a new partner, under pressure, or after consuming alcohol or drugs.
Unlike primary or secondary ED, it is usually short-term and linked to psychological or emotional triggers like performance anxiety or relationship stress.
Building trust with a partner and reducing stress levels often helps resolve it.
How Common Is ED?
ED is highly prevalent. By 2025, an estimated 322 million men globally will experience it, double the number from 1995. Around 50% of men aged 40–70 report some degree of ED.
Prevalence increases with age: 17% in men aged 40–49, 35% in those 50–59, 69% in their 60s, and over 80% in men aged 70 and older.
Causes of Erectile Dysfunction
ED can stem from physical, mental, or lifestyle-related issues; often, it’s a mix of all three.
Physical Causes of ED
Physical health plays a major role in ED.
Some common causes include:
Cardiovascular Issues
Heart and blood vessel health directly impact erectile function. Narrowed arteries from atherosclerosis, high blood pressure, or heart disease reduce blood flow to the penis, making it difficult to achieve or sustain an erection.
In many men, ED can be the first noticeable sign of underlying cardiovascular disease. Addressing these heart-related issues early can often improve or even reverse ED.
Diabetes and ED
Diabetes contributes to ED by damaging both blood vessels and nerves that are essential for erections.
Over time, high blood sugar impairs blood flow and nerve sensitivity, making arousal and erection harder to maintain.
Men with diabetes are up to three times more likely to experience ED than those without it, especially if their blood sugar is poorly controlled.
Hormonal Imbalances
Hormones like testosterone play a vital role in libido and sexual performance. Low testosterone, thyroid disorders, or elevated prolactin levels can all interfere with erectile function.
Symptoms might include low sex drive, fatigue, and reduced muscle mass. Hormone testing can help identify imbalances and guide proper treatment.
Neurological Disorders
The brain and nervous system control the sequence of events leading to an erection. Conditions like Parkinson’s disease, multiple sclerosis, stroke, or spinal cord injuries can disrupt these nerve signals.
When communication between the brain and genitals is impaired, ED often follows. Depending on the condition, treatment may involve physical therapy, medications, or assistive devices.
Psychological Causes of ED
Mental health is equally important:
Stress and Anxiety
Chronic stress, whether from work, finances, or personal life, can interfere with the brain’s ability to send the right signals to trigger an erection.
Performance anxiety, in particular, can create a cycle where fear of failure leads to continued difficulty with sexual performance. These psychological factors contribute to roughly 10–20% of ED cases.
Depression and ED
Depression can drain sexual desire and interfere with the physical response to arousal. It also affects energy levels, mood, and confidence, all of which are critical for sexual functioning.
Additionally, many common antidepressants (especially SSRIs) list ED as a side effect, compounding the issue.
Relationship Issues
Emotional disconnect, lack of communication, unresolved conflict, or tension in a relationship can manifest as sexual dysfunction.
When intimacy and trust are affected, ED can follow. Addressing these issues through open dialogue or couples therapy can lead to meaningful improvements.
Lifestyle Factors Contributing to ED
Every day habits play a big role in erectile health; some help it, others hurt it.
Smoking and ED
Smoking harms the inner lining of blood vessels and reduces nitric oxide, a key chemical needed for erections.
This limits blood flow to the penis, making it harder to achieve or maintain an erection. Quitting smoking can significantly improve erectile function, especially in younger men or those without other health conditions.
Alcohol Consumption
While moderate alcohol consumption may not affect sexual performance in most men, chronic heavy drinking is a different story.
It depresses the nervous system, disrupts hormone levels, and damages the liver, all of which can contribute to ED. Over time, alcohol-related nerve damage and reduced testosterone can make ED worse.
Poor Diet and Exercise
A diet high in processed foods, added sugars, and unhealthy fats contributes to obesity, diabetes, and vascular disease, all major ED risk factors.
On the other hand, regular physical activity and a balanced diet improve blood flow, support healthy hormone levels, and reduce inflammation. Men who exercise consistently may reduce their risk of ED by up to 60%.
Signs and Symptoms of ED
ED often starts with subtle changes; here’s what to watch for before it becomes more serious.
Early Warning Signs
Mild and occasional difficulties, such as softer erections or reduced sexual desire, may indicate early-stage ED.
Severity Levels of ED
- Mild: Occasional difficulty
- Moderate: Frequent problems maintaining an erection
- Severe: Rarely or never able to achieve an erection
Severity is often assessed using tools like the Sexual Health Inventory for Men (SHIM).
When Symptoms Become Concerning
If erection issues persist over weeks or months, or interfere with relationships or self-esteem, it’s time to seek help.
Accompanying symptoms like pain should also prompt medical attention.
Age and ED: What to Expect

ED doesn’t discriminate by age, but its causes and patterns often change as men get older.
According to a study published in the Journal of Sexual Medicine, ED affects about 26% of men under 40, with the prevalence rising to 40% by age 40 and 70% by age 70.
This highlights the importance of understanding how age-related factors like declining testosterone, chronic disease, and vascular changes influence erectile health.
ED in Young Men (20s–30s)
About 10–20% of young men experience ED.
In most cases, the cause is psychological or lifestyle-related, but in some cases is linked to conditions like diabetes or smoking.
ED in Middle-Aged Men (40s–50s)
Between 17–35% of men in their 40s and 50s report ED.
Causes tend to be a mix of physical decline, stress, and health conditions.
ED in Older Men (60+)
Between 69–83% of men aged 60+ have some form of ED, largely due to vascular decline, nerve damage, and chronic illness.
Source: https://pmc.ncbi.nlm.nih.gov/articles/PMC5313305/
Diagnosis of Erectile Dysfunction

Getting to the root of ED starts with the right diagnosis. Here’s how doctors figure out what’s going on.
When to See a Doctor
Men should consult a healthcare provider if ED is persistent, sudden, or accompanied by other health changes, especially in the presence of chronic illness.
Medical Tests for ED
Doctors use a range of tests to uncover what’s causing ED and guide the right treatment.
Blood Tests
Used to check for diabetes, hormonal levels, cholesterol, and kidney function.
Physical Examination
Doctors may check for signs of hormonal deficiency, blood pressure issues, or physical abnormalities.
Psychological Assessment
Screening for depression, anxiety, or relationship stress can help identify psychological contributors.
Self-Assessment Tools
Tools like the SHIM questionnaire help men evaluate severity. Though less commonly used now, tests like the Nocturnal Penile Tumescence (NPT) may still provide insights.
Treatment Options for ED
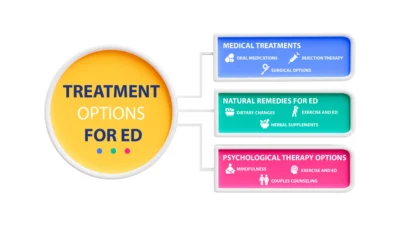
ED isn’t the end of the road; here’s how you can treat it with a mix of medical, natural, and psychological approaches.
Medical Treatments
These medical options are some of the most common and most effective ways to treat ED when lifestyle changes aren’t enough.
Oral Medications
PDE5 inhibitors (such as Viagra, Cialis, Levitra, and Stendra) work by relaxing blood vessels and increasing blood flow to the penis.
These medications are often taken before sexual activity and are effective for 60–80% of men.
They’re generally safe when prescribed, but may not be suitable for those taking nitrates or certain heart medications.
Injection Therapy
Alprostadil injections are used when pills are ineffective. This medication is injected directly into the base or side of the penis to trigger an erection within 5–20 minutes.
Although highly effective, some men may experience discomfort or bruising at the injection site.
Vacuum Devices
Vacuum erection devices (VEDs) create negative pressure around the penis, drawing blood into the tissue.
A constriction ring is placed at the base to maintain the erection.
About 80% of users find success with VEDs, especially those who want a non-drug option or have medical conditions that limit other treatments.
Surgical Options
Surgery is typically a last resort. Penile implants, either inflatable or semi-rigid, offer a permanent solution for men who haven’t had success with other treatments.
Vascular surgery, though rare, may be an option for younger men with specific blood flow blockages.
Natural Remedies for ED
If you’re looking for gentler alternatives, natural remedies can support better erections and overall sexual health.
Dietary Changes
Eating habits directly affect erectile function. A Mediterranean-style diet, rich in colorful vegetables, whole grains, legumes, lean protein (like fish and chicken), and healthy fats, supports heart and blood vessel health, which is crucial for strong erections.
Reducing sugar and processed foods helps maintain stable blood sugar and hormone levels.
Exercise and ED
Physical activity boosts circulation, supports testosterone production, and reduces stress.
Aerobic exercises like jogging or swimming improve heart health, while strength training helps balance hormones and build confidence. Aim for a routine that combines both for the best results.
Herbal Supplements
Some supplements like Panax ginseng, L-arginine, and yohimbine may support erectile function by improving blood flow or nerve signaling.
However, their effects can vary, and they may interact with medications. Always consult a doctor before using them.
Psychological Therapy Options
Mental and emotional well-being are key to sexual health. Cognitive-behavioral therapy (CBT) helps address performance anxiety and negative thought patterns.
Mindfulness-based approaches improve relaxation and presence. Couples counseling can also strengthen communication and intimacy, both of which play a major role in overcoming ED.
Lifestyle Changes to Improve ED
Simple lifestyle shifts can go a long way in improving erectile function and overall sexual health.
Diet and Nutrition for ED
What you eat plays a direct role in your sexual health. Reduce processed foods, sugar, and trans fats.
Focus instead on whole foods like leafy greens, berries, lean proteins, whole grains, and healthy fats such as olive oil or nuts. These support healthy blood vessels and hormone levels.
Exercise Programs for Better Sexual Health
Staying active improves blood flow, boosts testosterone, and reduces stress.
Aim for at least 150 minutes of moderate aerobic activity like brisk walking, swimming, or cycling each week, plus strength training twice a week for added benefits.
Stress Management Techniques
Stress causes a spike in cortisol and adrenaline, which can interfere with arousal and erections.
Use techniques like deep breathing, meditation, yoga, or cognitive-behavioral therapy to help keep your mind calm and your body responsive.
Sleep and ED Connection
Poor sleep, especially sleep apnea, can lower testosterone levels and increase the risk of ED. Aim for 7–9 hours of quality sleep per night.
Stick to a routine, limit screen time before bed, and treat any sleep disorders through a professional if needed.
ED and Relationships
ED doesn’t just affect the body; it can disrupt emotional connection, strain communication, and influence how men see themselves in a relationship.
Communicating with Your Partner
Open and honest conversations can reduce anxiety, clear up misunderstandings, and deepen intimacy.
Hiding the issue often causes more tension, while discussing it can strengthen your emotional bond and lead to shared solutions.
Impact on Mental Health
ED can trigger feelings of embarrassment, shame, or failure, which may evolve into anxiety or depression if left unaddressed.
Seeking support from a therapist or counselor can help manage these emotions and improve overall well-being.
Building Confidence
Confidence often takes a hit with ED, but it can be rebuilt.
Learning about ED, talking with supportive partners or professionals, and making small health improvements can help restore a sense of control and self-worth.
Prevention of Erectile Dysfunction
Good habits now can help prevent ED later. Here’s how to protect your sexual health long-term.
Healthy Lifestyle Habits
Avoid smoking, limit alcohol, eat a nutrient-rich diet, maintain a healthy weight, and stay physically active.
These habits support strong circulation and hormone balance, which are key for sexual function.
Regular Health Check-ups
Schedule routine visits to monitor blood pressure, cholesterol, blood sugar, and testosterone levels.
Early detection and management of health issues can prevent ED from developing or worsening.
Managing Underlying Conditions
Chronic conditions like diabetes, hypertension, obesity, and heart disease increase the risk of ED.
Work with your healthcare provider to manage these conditions through medication, lifestyle changes, or both. The better your overall health, the lower your ED risk.
Common Myths About ED
ED is surrounded by a lot of myths; let’s clear up the biggest ones with facts that hold up.
Misconceptions About Age
Myth: ED is inevitable with age.
Fact: While ED becomes more common as men grow older, it’s not guaranteed. Many men in their 60s and beyond continue to enjoy healthy sex lives by staying physically active, eating well, and managing chronic health conditions.
ED and Masculinity Myths
Myth: ED makes you less of a man.
Fact: ED is a medical issue, just like high blood pressure or diabetes, and it doesn’t define your masculinity. Seeking help is a sign of strength, not weakness.
Treatment Myths Debunked
Myth: Only pills or surgery work.
Fact: Medications are helpful, but they’re not the only option. Many men see major improvement through exercise, diet, therapy, and addressing underlying health issues. A holistic approach often brings the best results.
When to Seek Professional Help
Don’t wait until ED starts affecting your quality of life; early action matters. Seek professional help if symptoms are persistent, appear suddenly, cause emotional stress, or are linked with other health issues like chest pain, fatigue, or hormone changes.
A healthcare provider can identify the root cause and guide you through safe and effective treatment options.
Living with ED: Long-term Management
Living with ED doesn’t mean settling for less. Long-term management means staying on top of your physical and mental health.
Regular check-ups, maintaining a heart-healthy lifestyle, open communication with your partner, and possibly ongoing therapy can all make a big difference.
The key is consistency; small, steady efforts often lead to meaningful and lasting improvements in sexual health and confidence.
Conclusion
Erectile dysfunction is more than just a bedroom issue; it’s often a signal from your body that something deeper may be going on.
Whether caused by physical conditions, psychological factors, or lifestyle habits, ED is highly manageable with the right approach.
The good news? You’re not alone, and there are proven solutions available.
From medications and therapy to exercise and dietary improvements, taking action can significantly improve your sexual health and overall well-being.
Don’t wait for things to get worse; understanding your options and making proactive changes today can lead to a healthier, more confident future.
FAQs
Q: Is ED just a normal part of aging?
A: No. Age increases risk, but healthy habits can prevent or delay ED.
Q: Can young men get ED?
A: Yes. About 10–20% of young men experience ED, mostly from lifestyle or psychological causes.
Q: Can lifestyle changes help ED?
A: Absolutely. Diet, exercise, and stress reduction can significantly improve symptoms.
Q: Are treatments safe and effective?
A: Yes. Many options, from medications to therapy, offer proven benefits.
Q: Is ED linked to other health problems?
A: Often, yes. It can be an early sign of heart disease, diabetes, or hormonal issues. Get checked by a doctor.
Aug 12, 2025
Generic and brand name medications work the same. They treat the same conditions and use the same main ingredients. The big difference is price generics…
VIEW DETAILSAug 12, 2025
Fenbendazole is not considered safe for human use according to the FDA and major medical bodies. While some people are…
Aug 12, 2025
Semaglutide helps people lose weight by lowering hunger and making them feel full for longer. It’s available as a weekly…

